COVID-19 and Mucormycosis (black fungus)
COVID-19 and Mucormycosis (Black Fungus)
COVID-19 and Mucormycosis (black fungus), how are they related?
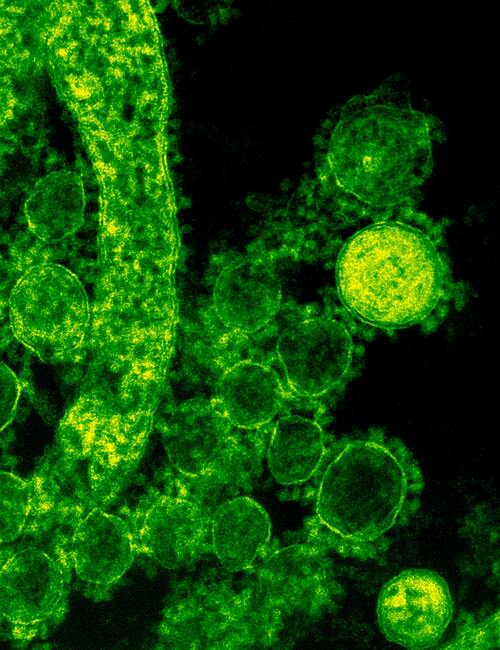
A group of molds known as mucormycetes leads to a scarce fungal infection which is called mucormycosis. How mucormycosis is related to those with COVID-19? the answer lies in the challenged immunity. People suffering from lowered immunity are susceptible to catching other infections as well, the same happens with the patients of COVID-19. Their weakened immune system attracts these black and sometimes lethal microorganisms. Those infected from COVID-19 are at higher risk of getting infected with black fungus because steroids used in the treatment of COVID-19 increase sugar levels and lower immunity.
On average around 50% of the infected people die due to complications and late treatment, chemotherapy is another reason for this. They can be cured but may prove to be deadly if not detected and controlled at an earlier stage. One can contract the fungus by inhaling the mold spores or they get into contact with them in things like soil, rotting produce or bread, etc.
Mucormycosis types and Symptoms
The symptoms vary depending upon the site of infection. In the case of rhinocerebral mucormycosis where the sinuses and brain get affected, the patient complains of headache, nasal or sinus congestion, one-sided facial swelling, black lesions on the nasal bridge or upper inside of the mouth.
In pulmonary mucormycosis – fever, cough, chest pain, and shortness of breath are observed. Cutaneous (skin) mucormycosis can look like blisters or ulcers, and the infected area may turn black. Other symptoms include pain, warmth, excessive redness, or swelling around a wound. Gastrointestinal mucormycosis includes abdominal pain, nausea, vomiting, gastrointestinal bleeding
Disseminated mucormycosis are seen in people who are already ill with other medical conditions. Such patients can develop mental status changes or even coma.
Who are at higher risk of catching mucormycosis?
People who are already suffering from diabetes, renal diseases, liver infections, old age, cardiac ailments, or patients who are on treatment for auto-immune disorders. And especially if they are or suffering or have survived the COVID-19.
Can mucormycosis be cured?
Mucormycosis can be treated with antifungal drugs like amphotericin B, isavuconazole, and Posaconazole. But again, it depends on the severity and the disease’s stage.
Side effects of the drugs used in the treatment of mucormycosis:
Drugs used in the treatment of mucormycosis have serious side effects and can cause kidney issues, neurological dysfunction, and sometimes stroke.